What happens to the brain when serotonin is lacking?
Serotonin deficiency affects more than just your mood—it can disrupt brain function, impact sleep, impair cognitive performance, and alter behavior. This comprehensive blog post explores the vital role serotonin plays in brain chemistry through the lens of emerging science highlighting the connection between gut health and mental wellness. We answer common questions about what happens when serotonin is lacking, how the gut microbiome contributes to serotonin production, and why gut microbiome testing may be key to identifying the root cause of chronic mood issues like anxiety and depression. If you're seeking clarity on serotonin's role in emotional balance and mental clarity, you'll find helpful insights here.
Introduction
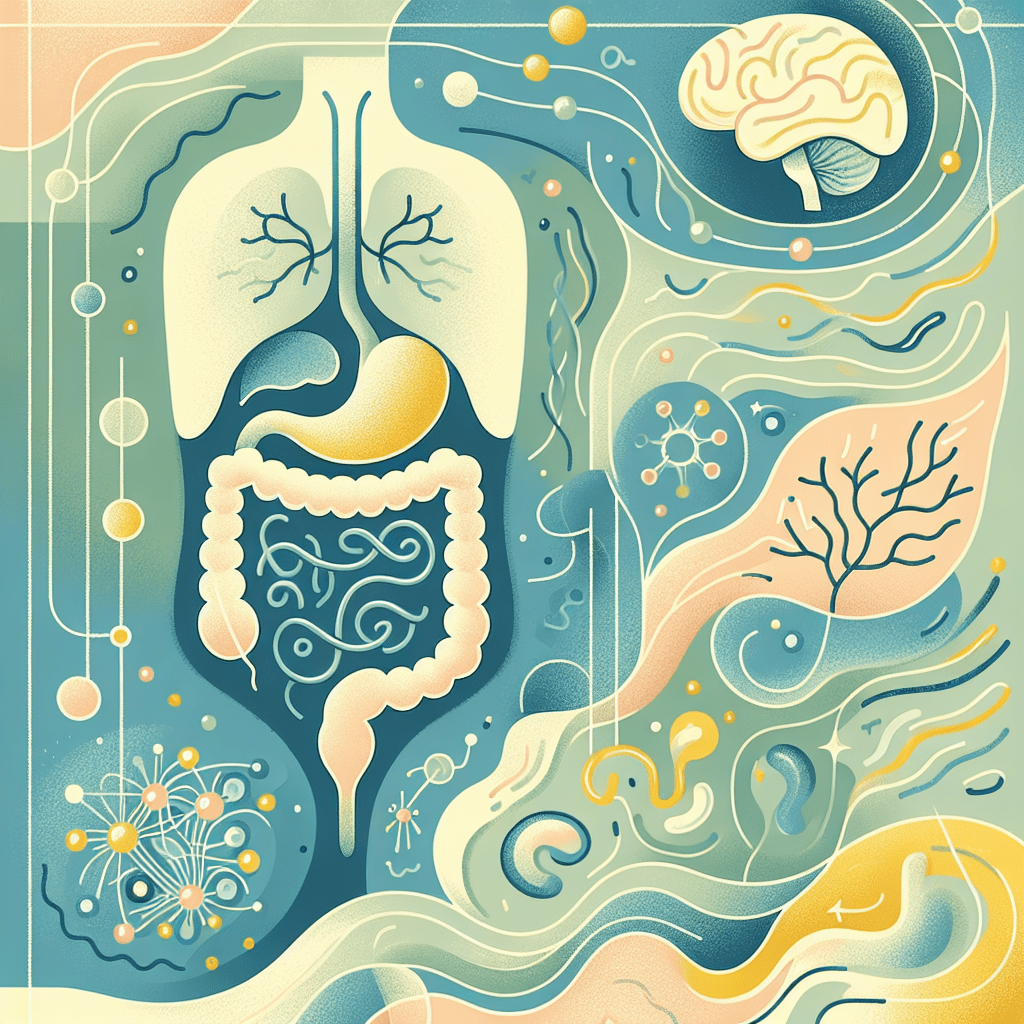
Serotonin, scientifically known as 5-hydroxytryptamine (5-HT), is a critical neurotransmitter involved in regulating mood, cognition, reward, learning, memory, and numerous physiological processes ranging from digestion to sleep cycles. Although it's often associated with mental wellbeing, roughly 90–95% of serotonin in your body is actually produced in the gastrointestinal (GI) tract. This fascinating fact opens a new realm of understanding: the strong, bidirectional communication between your gut and your brain, known as the gut-brain axis.
Emerging research suggests that the gut microbiome—comprising trillions of bacteria, fungi, viruses, and other microbes—plays a significant role in serotonin production. Certain beneficial gut bacteria even directly synthesize serotonin or influence its availability indirectly by affecting the metabolism of tryptophan, serotonin’s amino acid precursor. When an individual experiences serotonin deficiency, it may not just originate in the brain—it could be a consequence of disrupted gut microbial balance.
In the era of holistic health and personalized medicine, assessing one's microbiome via microbiome testing has become an important strategy. Companies such as InnerBuddies offer science-driven gut microbiome testing that can uncover bacterial imbalances or deficiencies associated with serotonin dysfunction. As we'll explore in this in-depth blog, restoring a healthy microbiome offers a promising route to improving brain function, mental health, and overall wellbeing.
I. The Impact of Serotonin Deficiency on Gut Microbiome Testing
To fully grasp the interplay between serotonin and the microbiome, it’s important to understand how the absence of serotonin affects gut health, and how gut health assessments like microbiome testing can provide critical insights. There’s a dynamic feedback loop between the brain's serotonin levels and the community of bacteria living in your digestive tract—one that, when thrown out of balance, can set the stage for long-term mental and physical challenges.
Various studies have shown that low serotonin levels can negatively impact the diversity and volume of beneficial gut bacteria. Reduced serotonin availability may impede the gut’s ability to regulate motility (the natural movements that push food through the intestines), reduce intestinal secretion, and compromise immune response within the intestinal mucosa. These disturbances reshape the environment of the gastrointestinal tract, often reducing populations of health-promoting microbes such as Lactobacillus and Bifidobacterium.
In turn, these microbial imbalances can reduce the microbial species that are directly or indirectly involved in serotonin synthesis. For instance, some gut bacteria facilitate the production of short-chain fatty acids (SCFAs), which play an essential role in producing the serotonin precursor tryptophan. When these helpful microbes dwindle, less tryptophan is available for conversion, leading to even lower serotonin levels, effectively creating a vicious cycle of deficiency.
Enter gut microbiome testing—a powerful diagnostic tool that allows clinicians and individuals to better understand what’s happening inside their gut. Through the analysis of stool samples, tests like the InnerBuddies Gut Microbiome Test identify the presence and abundance of various microbial species. If testing reveals a lack of serotonin-promoting bacteria or overgrowth of pathogenic microbes, it points to the gut as a probable contributor to serotonin deficiency and the accompanying neurological or psychological symptoms.
Armed with this data, individuals can embark on targeted therapies—ranging from probiotic supplementation to dietary interventions—designed to rebalance the microbiome and, in turn, support serotonin production. As a result, gut microbiome testing represents more than a wellness trend; it’s an essential step in uncovering and addressing the hidden biological causes behind serotonin-related disorders.
II. Neurotransmitter Imbalance and Its Effect on Brain Function
Serotonin is one of several key neurotransmitters that regulate brain function and behavior. Alongside dopamine, gamma-aminobutyric acid (GABA), and norepinephrine, serotonin contributes to a delicate biochemical symphony in your central nervous system. A deficiency in serotonin doesn’t merely cause a drop in mood—it disrupts the broader neurotransmitter network, with serious consequences for mental clarity, emotional resilience, and even motor coordination.
Serotonin is directly involved in the balance between excitatory and inhibitory signaling in the brain. For instance, it works alongside GABA to produce calming effects. When serotonin levels fall, GABA's effectiveness may diminish, leading to heightened anxiety or symptoms resembling attention-deficit/hyperactivity disorder (ADHD). Similarly, low serotonin can affect dopamine transmission by interfering with reward processing and motivation—two cognitive domains where dopamine is especially influential.
This disruption at the neurochemical level affects a range of neural communication pathways. Synaptic plasticity—the brain's ability to strengthen or weaken synapses based on experience—is hampered when serotonin is low. Over time, reduced nerve signaling efficiency can contribute to memory lapses, difficulty concentrating, obsessive thoughts, and impaired decision-making abilities. Taken together, these effects highlight why serotonin imbalance should be recognized as a multidimensional brain health issue, not merely a mood disorder symptom.
The gut microbiome, again, plays a starring role in this drama. Gut bacteria manage the synthesis and regulation of multiple neurotransmitters. For instance, species like Bacillus and Escherichia can produce dopamine, while certain strains of Lactobacillus help optimize GABA production. When microbial diversity diminishes, the synthesis of these vital neurochemicals declines alongside serotonin.
Regular gut microbiome testing can identify whether dysbiosis is impairing neurotransmitter production or signaling. This can be particularly helpful for those struggling with persistent cognitive fog, anxiety, or mood instability. Rather than masking symptoms with medications alone, testing allows for personalized treatments that restore the body’s ability to produce neurotransmitters naturally.
III. Serotonin Levels Impact Mood, Appetite, and Sleep Patterns
The triad of mood, appetite, and sleep forms the foundation of human wellbeing. Unsurprisingly, serotonin plays an integral role in regulating all three processes. A deficiency in this neurotransmitter can unravel emotional equilibrium, interfere with hunger signals, and disrupt the body's internal clock, leading to sleep disorders and chronic fatigue.
As a modulator of emotional regulation, serotonin functions by stabilizing mood and providing feelings of contentment. When serotonin levels decline, people may experience increased sadness, agitation, or general dysphoria. Feelings of worry or uncontrollable anxiety may arise—often without clear cause—a condition sometimes referred to as “brain-based anxiety.” Mood swings, irritability, and low self-esteem are also common in those affected by deficient serotonin signaling.
Serotonin also governs satiety—the sensation of fullness—by acting on receptors in the hypothalamus and digestive system. In serotonin-deficient individuals, abnormal appetite regulation often occurs, leading to overeating or undereating. Cravings for carbohydrates, sweets, or salty snacks may appear more frequently due to the temporary serotonin-boosting effects of these foods. This behavior not only exacerbates gut dysbiosis but also contributes to blood sugar imbalances and subsequent mood disturbances.
Sleep, too, is disturbed when serotonin is lacking. This neurotransmitter is a precursor to melatonin, the hormone that regulates circadian rhythms. Without sufficient serotonin, the brain struggles to create enough melatonin to maintain healthy sleep cycles. Individuals may have difficulty falling asleep, experience frequent night awakenings, or wake up feeling unrested. Over time, chronic sleep disturbances further affect serotonin regulation, completing a feedback loop that worsens symptoms.
The gut microbiome again proves crucial in maintaining balance across mood, appetite, and sleep. Disruptions in the gut-brain axis caused by microbial imbalances can reduce the conversion efficiency of tryptophan into serotonin. Through gut microbiome testing, these imbalances can be detected and corrected using prebiotic and probiotic strategies, dietary modifications, and mindfulness-based stress reduction, restoring equilibrium naturally.
IV. Mood Regulation Deficits: From Anxiety to Depression
Serotonin deficiency has long been implicated in the pathogenesis of mood disorders such as generalized anxiety disorder (GAD), major depressive disorder (MDD), and dysthymia. Although the exact causes of these conditions are multifactorial—ranging from genetic to environmental triggers—the central role of serotonin in mood regulation remains consistent across diagnostic criteria and research literature.
Low serotonin affects neural circuits involved in emotional processing, particularly structures like the amygdala and prefrontal cortex. In individuals with anxiety or depression, these circuits are hyperactive or dysfunctional, often leading to negative thought patterns, excessive rumination, and low motivation. This biological substrate explains why serotonin-targeted medications like selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to treat these ailments.
However, evidence increasingly suggests that mood disorders may stem not only from brain-centric processes but also from imbalances in the gut. Gut microbiome dysbiosis has been observed in numerous patients with mood disorders. High levels of pro-inflammatory microbial strains and low levels of anti-inflammatory, serotonin-producing bacteria are hallmarks in many of these cases.
Recent studies have demonstrated that restoring gut microbial balance using probiotics, prebiotics, and dietary interventions can alleviate symptoms of both depression and anxiety. Strategies include increasing fiber-rich foods, reducing sugar and processed foods, and supplementing with strains like Lactobacillus rhamnosus or Bifidobacterium longum. These microbes not only modulate immune and stress responses but also actively participate in serotonin metabolism.
As more clinicians turn toward integrative and person-centered mental health approaches, microbiome testing is becoming central to forming a personalized action plan. By pinpointing gut imbalances that may underlie mood regulation issues, such testing allows for tailored interventions that address root causes rather than merely managing surface symptoms.
V. Brain Chemistry Changes: From Neuroplasticity to Cognitive Function
Neuroplasticity refers to the brain's ability to change and adapt in response to new experiences, stimuli, damage, or learning. Serotonin is a vital driver of this process, especially in regions like the hippocampus—the brain’s learning and memory hub. When serotonin signaling is impaired due to deficiency, neuroplasticity weakens, setting the stage for cognitive decline and impaired resilience to stress or trauma.
Low serotonin levels are associated with structural and functional changes in the brain. Dendritic branching—the growth of neural extensions that support synaptic connections—may be stunted, and growth factors like brain-derived neurotrophic factor (BDNF) are downregulated. These deficits result in poor learning ability, weaker memory recall, delayed decision-making, and reduced coping capacity in the face of life’s challenges.
The gut microbiome once again plays an influential role. Exposure to certain probiotics has been shown to elevate BDNF levels and restore neurogenesis in animal models. Microbial metabolites such as SCFAs trigger anti-inflammatory pathways that protect neural tissue and promote regeneration. Disrupted gut ecosystems, on the other hand, increase systemic inflammation and oxidative stress, both of which contribute to neurodegeneration and serotonin depletion.
Using gut microbiome testing, individuals can assess whether their cognitive fog, forgetfulness, or executive dysfunction may be tied to dysbiosis. Rebalancing the microbial environment through nutrition, targeted supplementation, and lifestyle modifications can potentially reverse early cognitive impairments and support long-term brain health—much of which hinges on serotonin optimization.
VI. Mental Health Effects of Serotonin Deficiency and Gut Microbiome Health
Beyond clinical diagnoses like anxiety and depression, serotonin deficiency can manifest in an array of subtler but still debilitating mental health symptoms, including chronic stress, irritability, emotional reactivity, lack of motivation, and even physical symptoms like fatigue and muscle tension.
Chronic stress further disrupts the microbiome by increasing cortisol, which dampens the growth of balanced microbial communities and suppresses serotonin-related gene expression. The more stressed you become, the worse your gut health—and serotonin levels—may become, creating a loop that perpetuates poor mood and energy regulation.
Reversing this pattern is possible through science-backed interventions. Microbiome testing is often the first step toward personalized healing. Tests like the InnerBuddies Gut Microbiome Test identify microbial profiles indicative of serotonin dysfunction. Armed with these insights, practitioners recommend precise probiotics, fermented foods, fiber-based prebiotics, and anti-inflammatory protocols.
When integrated with non-dietary strategies such as meditation, exercise, and therapy, these interventions offer a holistic toolkit for long-term serotonin restoration. Thus, the combination of microbiome insights with mental health support represents a promising frontier in reversing serotonin deficiency and rebalancing mood and cognition.
Conclusion
Serotonin plays a pivotal role in the harmonious functioning of the brain and body. When its levels waver, everything from neurotransmitter balance and mood to sleep, appetite, and cognitive ability can be thrown off course. Increasingly, the focus of science and medicine has turned to an unexpected yet deeply connected player in serotonin health—the gut microbiome.
By understanding this gut-brain synergy, proactive testing and targeted intervention become essential. Tools like gut microbiome tests from InnerBuddies provide actionable insights that not only explain persistent mental health symptoms but also guide safe and natural treatment paths.
Moving forward, the future of emotional wellbeing and optimized brain health is undeniably rooted in personalized, inside-out approaches. Addressing serotonin deficiency through gut microbiome testing and intervention is more than possible—it's proving transformative.
Q&A Section
Q: What is serotonin deficiency?
A: Serotonin deficiency refers to reduced levels or function of serotonin, a key neurotransmitter essential for mood regulation, cognition, appetite, and sleep.
Q: What causes serotonin levels to decrease?
A: Factors include poor gut health, chronic stress, genetic predisposition, inadequate dietary intake of tryptophan, and disordered gut microbiota.
Q: How does gut microbiome affect serotonin?
A: Certain gut bacteria help synthesize or regulate serotonin through the metabolism of tryptophan. A healthy microbiome supports serotonin production and signaling.
Q: Can microbiome testing help with serotonin-related issues?
A: Yes. Gut microbiome testing, such as the one offered by InnerBuddies, can identify microbial imbalances that may contribute to serotonin deficiency and offer targeted solutions.
Q: What are the natural ways to improve serotonin levels?
A: Regular exercise, exposure to sunlight, a nutrient-rich and fiber-packed diet, reduced stress, and microbiome-based interventions can all raise serotonin safely and effectively.
Important Keywords
serotonin deficiency, gut microbiome, microbiome testing, mood disorders, anxiety, depression, tryptophan, dopamine, GABA, neuroplasticity, emotional regulation, cognitive function, InnerBuddies gut test, gut-brain axis, probiotics for serotonin, brain health, serotonin and sleep, serotonin and appetite, mental health testing, personalized nutrition