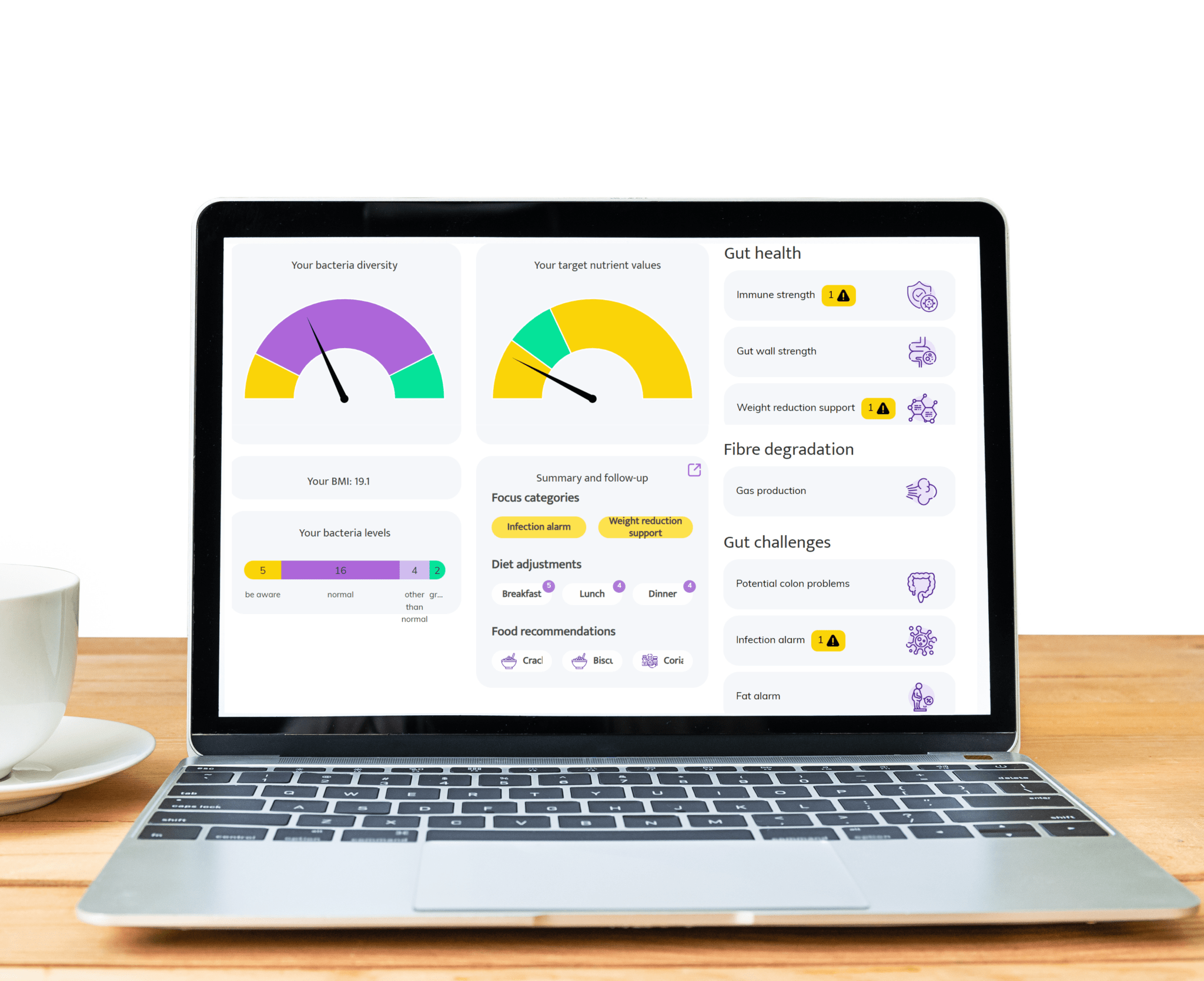
Recent research has revealed a strong connection between Irritable Bowel Syndrome (IBS) and the gut microbiome—the diverse community of bacteria, viruses, fungi, and other microbes living in the digestive tract. In healthy individuals, this microbiome plays a crucial role in digestion, immune function, and even mood regulation. However, in people with IBS, studies have found significant differences in the composition and activity of these gut microbes. For example, IBS patients often have lower levels of beneficial bacteria like Bifidobacterium and Lactobacillus, and higher levels of potentially harmful or pro-inflammatory species. These imbalances, known as dysbiosis, can disrupt the gut’s normal functions, leading to symptoms such as bloating, pain, and irregular bowel movements.
The mechanisms linking the microbiome to IBS symptoms are complex and multifaceted. One major pathway involves the production of short-chain fatty acids (SCFAs) and other microbial metabolites, which help regulate gut motility and inflammation. An altered microbiome may produce excessive gas or irritants, which can stimulate the gut’s nerve endings and trigger pain or urgency. Moreover, the gut-brain axis—a bidirectional communication system between the gut and central nervous system—can be influenced by microbial signals, potentially heightening sensitivity to normal digestive processes in IBS sufferers. These insights have opened new avenues for treatment, such as probiotics, prebiotics, dietary changes like the low-FODMAP diet, and even fecal microbiota transplantation, though more research is needed to fully understand and harness these approaches.