Which chemical are you lacking in depression?
Understanding depression requires more than focusing solely on the brain. As research into gut-brain communication grows, a clearer picture is emerging about the relationship between gut health and mental wellness — especially the role of gut bacteria in producing depression chemicals such as serotonin, dopamine, GABA, and norepinephrine. This blog post addresses which chemical deficiencies may play a role in depression and how gut microbiome testing can help detect and correct them. We explore the science behind gut-produced neurotransmitters and how personalized approaches based on microbiome profiles can support better mental health outcomes. Gut testing could hold the key to balanced moods and more effective treatments.
Depression Chemicals and Gut Microbiome Testing: The Key Players
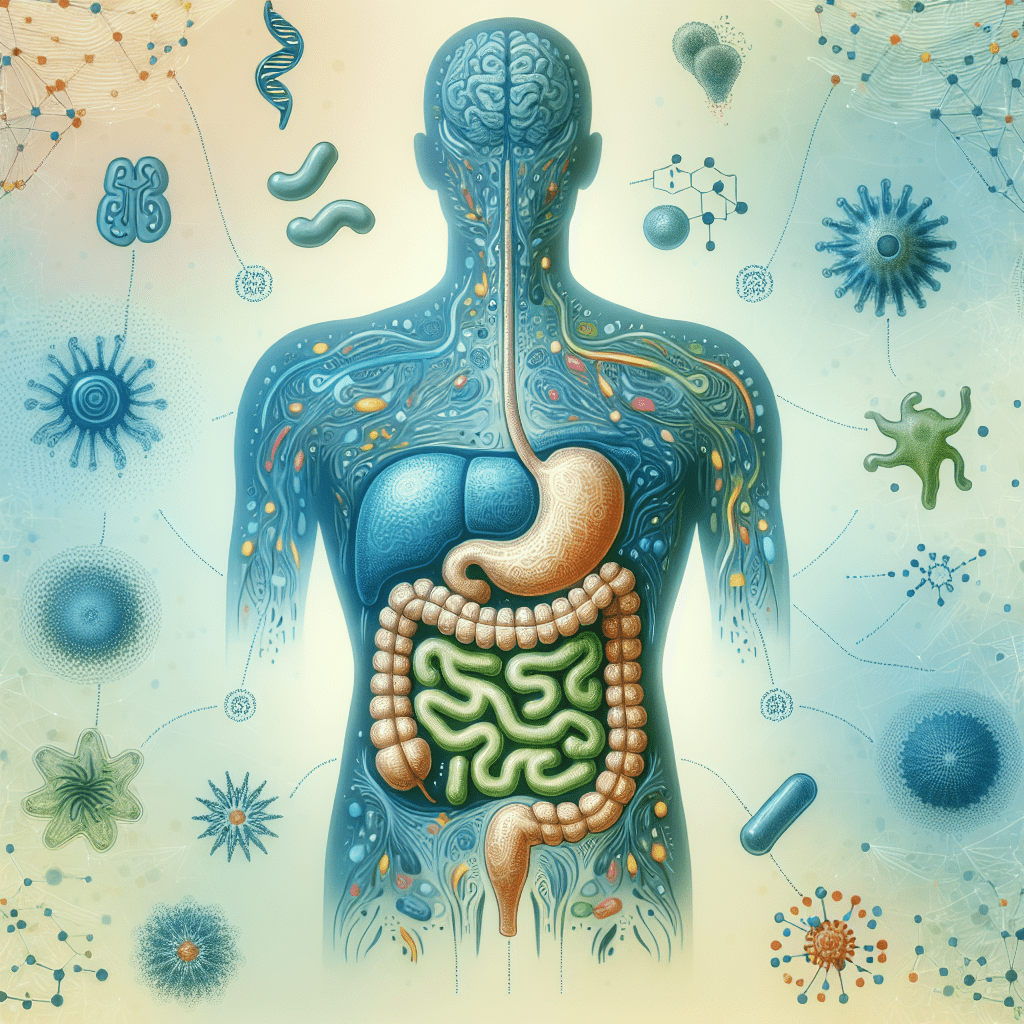
For decades, depression has been viewed primarily as a brain issue. A chemical imbalance theory has dominated much of the discussion, focusing on mood-regulating compounds like serotonin, dopamine, norepinephrine, and gamma-aminobutyric acid (GABA). While these neurotransmitters certainly play critical roles, recent advances in neuroscience and microbiology point to a more interconnected system — known as the gut-brain axis — where gut bacteria significantly influence brain chemistry.
Key depression chemicals include:
- Serotonin: Often referred to as the "feel-good" neurotransmitter, serotonin regulates mood, appetite, and sleep. Low levels are frequently associated with anxiety and depression.
- Dopamine: This neurotransmitter is essential for motivation, pleasure, and reward-seeking behaviors. Imbalances are linked to feelings of apathy, fatigue, and low focus.
- GABA: GABA is the brain's primary inhibitory neurotransmitter. It helps reduce neuronal excitability and manage stress. A deficiency may lead to anxiety and sleep disruption.
- Norepinephrine: A stress-response and arousal hormone that affects concentration and energy. Dysregulation is often observed in both depressive and anxious states.
Interestingly, the gut microbiome — the community of trillions of bacteria residing in our intestines — plays a pivotal role in the production and regulation of these neurotransmitters. Various strains of gut bacteria are involved in synthesizing these molecules or influencing their expression through metabolite signaling. The implication? An imbalance in gut microbiota can directly impact the levels of key neurotransmitters related to mood.
This understanding has made gut microbiome testing an indispensable tool in the personalized care of depression. Such tests analyze the diversity and composition of your gut flora, identifying any deficiencies or overgrowths that could be leading to low levels of depression chemicals. For example, an overgrowth of pro-inflammatory bacteria may disrupt serotonin production or impair the vagus nerve’s communication from gut to brain.
By mapping out the microbial ecosystem inside your gut, practitioners can develop targeted interventions. These may include probiotics, dietary changes, or even psychological therapies tailored to your gut-brain profile. In other words, depression might not begin in the brain — it could begin in the gut. Such revelations are revolutionizing how we identify depression's biological signatures and restore mental health with science-backed precision.
Neurotransmitter Deficiencies and Gut Health: Unlocking Mood with Microbiome Insights
Understanding how neurotransmitter deficiencies arise is fundamental to tackling depression at its root. Often, low mood is the surface symptom of complex biochemical issues occurring quietly within the body, particularly in the gut. The gut microbiome plays a crucial role in synthesizing and regulating neurotransmitters, turning what once seemed like separate bodily systems into highly interconnected biological pathways.
Serotonin, for example, is largely produced in the gut — roughly 90% of it. It is synthesized from tryptophan, an essential amino acid obtained from food. However, the successful conversion of tryptophan into serotonin relies heavily on the presence of certain gut bacteria. Microbes such as Bifidobacterium infantis and Lactobacillus plantarum help facilitate this conversion and regulate its balance through immune and metabolic pathways.
Similarly, dopamine — critical for regulating emotions, motor control, and cognition — is influenced by the gut microbiome. Specific bacteria can increase precursor compounds of dopamine, such as tyrosine and phenylalanine. Additionally, a balanced gut ecosystem supports a healthy blood-brain barrier and proper nutrient absorption, essential for neurotransmitter stability across both central and enteric nervous systems.
This is where microbiome testing becomes transformative. The test examines microbial communities in your gut, pointing out any lack of diversity, harmful overgrowth, or beneficial deficiencies that may contribute to poor neurotransmitter production. Testing can reveal dysbiosis — an unhealthy microbial imbalance — which has been empirically linked to reductions in serotonin, dopamine, and even brain-derived neurotrophic factor (BDNF), which affects overall brain plasticity and resilience.
Emerging studies also suggest that inflammation from bacterial imbalances can lead to increased permeability of the gut and brain barriers. This "leaky gut" phenomenon introduces toxins into the system, eliciting immune responses that interfere with nutrient synthesis and neurotransmitter conversion. Consequently, these systemic changes directly affect one's mood, stress tolerance, and outlook on life.
Detecting these imbalances early allows health providers and patients alike to intervene proactively. Custom protocols based on microbiome data can include targeted probiotics, prebiotics, vitamin supplementation (like B6, zinc, and magnesium essential for neurotransmitter formation), and lifestylistic shifts such as meditation and improved diet. The insights from microbiome testing bring mental health care closer to the realm of preventive medicine — a breakthrough in truly treating root causes, not just masking symptoms.
Mood Regulation Chemicals and the Gut Microbiome: Restoring Balance Naturally
Balancing mood over time involves maintaining appropriate levels of neurotransmitters within a flexible, responsive biology. While medications like SSRIs aim to adjust serotonin reuptake chemically, a more holistic approach is emerging — one that addresses the source of deficiency rather than simply regulating the outcome. And that source may very well be in your gut.
The gut microbiome's influence on mood includes a wide spectrum of chemicals crucial for mood equilibrium. Gamma-aminobutyric acid (GABA), for instance, provides calming effects that counterbalance excitatory responses in the brain. Deficiency in GABA is associated with heightened anxiety, restlessness, insomnia, and even depression. Gut strains such as Lactobacillus rhamnosus and Bifidobacterium longum have demonstrated the capacity to naturally produce GABA as part of the microbial metabolic process.
Similarly, norepinephrine — a neurotransmitter and hormone tied to alertness and attention — can suffer due to poor gut health. Fragmented microbiomes may have difficulty maintaining efficient norepinephrine recycling, contributing to fatigue, pessimism, and symptoms of mental "fog." Other neurochemicals, including peptide hormones and endorphins, also have interactive pathways reliant on gut microbiota for biosynthesis, regulation, and signaling.
Innovative gut microbiome tests help identify imbalances in these pathways. Typically, these tests analyze the presence of microbial metabolites such as short-chain fatty acids (SCFAs), which positively influence neurotransmitter levels and inflammation regulation. Butyrate, an SCFA produced by bacteria like Faecalibacterium prausnitzii, has neuroprotective effects and improves the gut barrier function — both vital to mental balance.
Restoring mood regulation chemicals doesn’t always require pharmaceuticals. By supporting beneficial bacteria through nutrition, targeted supplementation, and stress-reducing activities, you can encourage natural neurochemical regulation. Foods rich in fiber, polyphenols, fermented ingredients, and omega-3 fatty acids promote populations of neuromodulating bacteria. Additionally, lifestyle shifts such as sleep optimization, therapy, journaling, and daily exercise reinforce the effectiveness of dietary efforts.
Combined, these natural interventions may help recalibrate your body's internal chemistry. Microbiome-informed care means your personal gut data shape your mental wellness protocol — a forward-thinking strategy that replaces generic treatment with precision mental health support. Using microbiome insights to influence mood-regulating chemicals can deepen emotional resilience and trigger a longer-lasting sense of well-being.
Serotonin Levels and Gut Microflora: The Serotonin-Gut Connection
No conversation about depression chemicals is complete without a thorough exploration of serotonin — the neurotransmitter most commonly linked to mood, emotional processing, and satisfaction. While traditional treatments focus on increasing serotonin availability in the brain, a paradigm shift is highlighting the gut as serotonin’s primary production site. Roughly 90% of the body's serotonin is synthesized in the gastrointestinal tract, managed predominantly by enterochromaffin cells under the influence of specific gut bacteria.
These bacteria play a dual role: they both produce precursors to serotonin and stimulate host cells to produce it. Certain microbial strains, such as Bifidobacterium infantis and Streptococcus species, are known to enhance serotonin bioavailability by influencing pathways in the enteric nervous system. Additionally, bacterial metabolites like SCFAs influence tryptophan metabolism, enhancing serotonin synthesis in the gut environment.
When your microbiome is compromised — experiencing loss of beneficial strains or dominance by pathogenic bacteria — serotonin production can falter. This can manifest as mood disorders, sleep disturbances, tension, and increased vulnerability to stress. By using microbiome testing, health professionals can pinpoint deficits in serotonin-producing bacteria and highlight strategies to rebalance your internal ecosystem.
The insights from your gut profile can inform a range of interventions. For example, increasing consumption of tryptophan-rich foods like eggs, turkey, and cheese may be more effective when paired with prebiotics that feed serotonin-enhancing bacteria. Probiotic supplementation with specifically identified strains can also restore serotonin-producing balance, especially when driven by testing data.
This microbiome-serotonin connection doesn’t suggest discarding traditional antidepressants but rather strengthens treatment efficacy when paired with root cause analysis. Together, SSRIs and gut-focused interventions can enhance serotonin modulation systemically, rather than relying on the brain alone to pick up the slack. Testing can be done proactively — even before mood issues emerge — fortifying your mental health by supporting the gut’s vast influence on emotional regulation.
Dopamine Imbalance and Gut Microbiome: Understanding the Reward System
Dopamine is a key player in our reward system, driving motivation, satisfaction, and focus. It’s also directly implicated in various mental disorders, from depression and anxiety to addiction and ADHD. Too little dopamine can result in apathy, low energy, and diminished ability to feel joy — hallmark symptoms of depressive episodes. Surprisingly, your gut has a big say in how much dopamine is circulating in your body.
Several types of beneficial bacteria can produce the precursors required for dopamine synthesis. For instance, strains like Bacillus and Lactobacillus generate tyrosine, a building block of dopamine. Moreover, they can regulate enzymes such as tyrosine hydroxylase, which plays a role in the dopamine production pathway. These bacteria also influence how dopamine receptors function through complex molecular signaling mechanisms.
When an individual's gut microbiota is compromised (termed dysbiosis), dopamine-related functions suffer. The breakdown in communication between the gut and brain, oxidative stress, and inflammation caused by gut imbalances can all degrade dopaminergic pathways. Through advanced microbiome analysis, it's now possible to detect which bacterial strains are missing or underrepresented in your intestinal environment — and correct them before they create downstream mental health effects.
Healing your dopamine system through microbiome-focused strategies might involve tailored probiotics, amino acid supplementation (like phenylalanine), and avoiding inflammatory foods that interrupt the integrity of the gut barrier. Moderate physical activity and exposure to sunlight further enhance dopamine turnover, particularly when gut health is working in harmony with lifestyle.
People with depression connected to dopamine imbalance often describe their world as muted, drained of enthusiasm or purpose. Biochemical data now allows us to find tangible reasons for these experiences beyond abstract psychological theories. Embracing a gut-brain strategy provides a new framework for tackling depression from the inside out — grounded in science, measurable progress, and personal biological insight.
Neurotransmitter Therapy and Gut Microbiome: Personalized Approaches to Mental Well-being
With the intricate relationship between gut microbiome and neurotransmitters established, the next frontier is applying this knowledge to therapy. Healthcare is shifting toward more individualized, biology-driven treatments, and nowhere is this clearer than in the merging of mental well-being and microbiome science. Tailored neurotransmitter therapy based on gut microbiota composition is gaining traction as an effective strategy for depression management.
Neurotransmitter therapy refers to targeted attempts to restore balance in brain chemical systems. This may include:
- Supplementation with amino acid precursors like 5-HTP, tyrosine, and GABA
- High-quality probiotics designed to enhance specific neurotransmitter production
- Personalized nutrition plans based on gut testing data
- Functional foods and fiber that support healthy bacteria growth
Microbiome testing plays a pivotal role by clearly identifying what microbial support your body needs. Instead of general dietary advice or guesswork, you receive precise, data-driven insights on which neurotransmitter systems are imbalanced — and which gut interventions can help regulate them.
Future therapies may even use genetically engineered probiotics or fecal transplants tailored to foster dopamine or serotonin-producing bacteria. We’re only beginning to harness the full potential of microbiome insights, but the promise is enormous: safer, more sustainable treatments with fewer side effects and more long-term impact than traditional pharmaceuticals alone.
Most importantly, neurotransmitter therapy supported by microbiome diagnostics acknowledges the individual nature of depression. No two bodies — or guts — are alike. Empowering patients to understand their internal ecosystem offers a revolutionary approach to managing mental health, giving hope not just for symptom management, but full recovery.
Conclusion
The intersection of gut health and mental health is more than just an academic interest — it’s transforming how we approach treatment for depression and other mood disorders. The evidence is clear: the gut microbiome plays a crucial role in regulating depression chemicals like serotonin, dopamine, GABA, and norepinephrine. When your microbial ecosystem is imbalanced, your mood, energy, focus, and well-being can all suffer.
Thanks to advanced gut microbiome testing, we now have the tools to uncover chemical imbalances that start in the gut. Personalized, gut-based approaches provide targeted pathways to restore mental equilibrium naturally, breaking free from the one-size-fits-all mold of conventional depression treatment.
If you've struggled to find lasting relief from mood swings, lack of motivation, or chronic stress, it might be time to look within — right into your gut. Consider integrating gut microbiome testing into your wellness plan and unlock a new dimension of personalized mental health care grounded in proven science.
Q&A Section
Which chemicals are most involved in depression?
The primary depression chemicals include serotonin, dopamine, GABA, and norepinephrine. These neurotransmitters influence mood, motivation, focus, and stress responses.
How is the gut microbiome connected to these chemicals?
Gut bacteria help synthesize or regulate the availability of these chemicals. Imbalances in gut flora can lead to neurotransmitter deficiencies and depressive symptoms.
Can gut microbiome testing actually help improve mental health?
Yes. Gut microbiome testing provides insight into microbial imbalances that may be affecting your mood-regulating neurotransmitters, allowing practitioners to recommend targeted interventions.
What are some natural ways to support neurotransmitter production through gut health?
Eating a high-fiber, whole-food diet, taking targeted probiotics, reducing stress, sleeping well, and supplementing with amino acids like tryptophan and tyrosine can help support neurotransmitter balance naturally.
Where can I get a gut microbiome test?
You can explore a comprehensive gut health solution through InnerBuddies' gut microbiome test, designed to provide personalized data on your microbial profile and mental health connections.
Important Keywords
- depression chemicals
- gut microbiome testing
- serotonin and gut connection
- dopamine imbalance
- neurotransmitter deficiencies
- gut-brain axis
- personalized mental health treatment
- GABA gut bacteria
- norepinephrine and mood
- InnerBuddies microbiome test